How to: assess patient suitability for unlicensed phage therapy in the United Kingdom
Phage therapy may be used as an unlicensed medicine in the United Kingdom
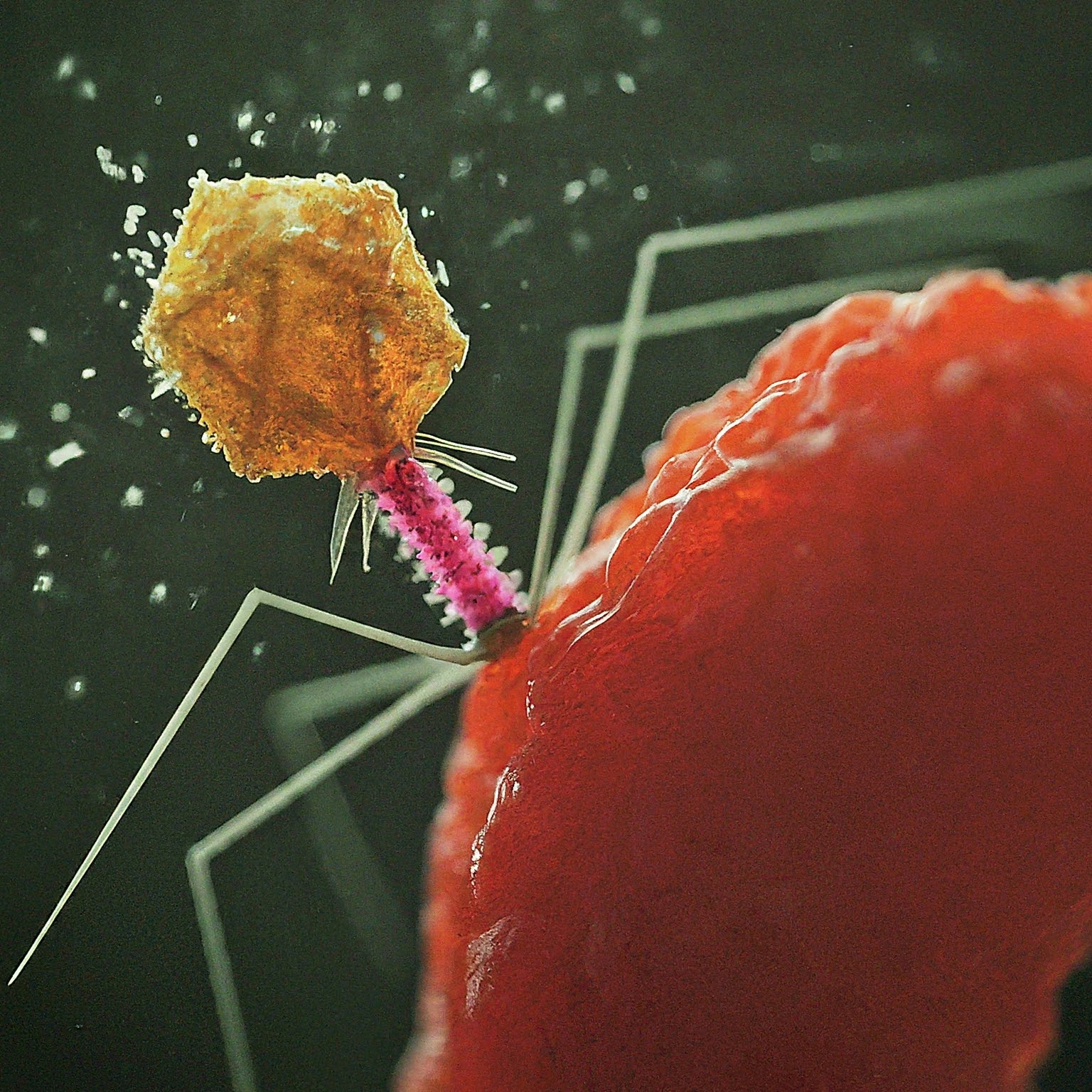
Naturally occurring phages are classified by the UK’s Medicine’s and Health care Product’s Regulatory Agency (MHRA) as biological medicines. MHRA guidance states that unlicensed medicines, such as phages, may be considered to meet special clinical needs and that responsibility for deciding whether an individual patient has special needs, which a licensed product cannot meet, should be a matter for the doctor (or other health care professional) responsible for the patient’s care’. Health Improvement Scotland’s (HIS) recommendation for the consideration of phage therapy in difficult-to-treat infections similarly states that phage therapy may be considered at the discretion of the responsible clinician. The UK’s NHS is comprised of discrete local health authorities known as NHS Trusts. Unlicensed medicines (ULMs) are widely used in the NHS, and consequently, all NHS Trusts have local policies and procedures for governing ULM use.
Patient suitability should be assessed through existing clinical pathways
Health Improvement Scotland’s recommendation for the consideration of phage therapy in difficult-to-treat infections defined four broad categories of patient suitability; these categories are shown in Table 1, alongside examples from our practice. The breadth of these categories is important because the unlicensed use of phage therapy will be suitable for a wide range of unique cases. Consequently, a narrower or more stringent classification of suitability, even within one speciality, risks erroneously excluding patients that may benefit. Read more here.
Table 1. Patient suitability for phage therapy
| Category | Example(s) from our practice |
|---|---|
| Antibiotic resistance | • Hip infection caused by a pan-resistant Bacteroides fragilis • Substernal abscess caused by pan-resistant methicillin resistant Staphylococcus aureus |
| Antibiotic sensitivity but clinical recalcitrance | • Prosthetic joint infection caused by Klebsiella pneumoniae biofilm on retained metalwork • Metal neurosurgical stabilisation device chronically colonised with Pseudomonas aeruginosa |
| High risk of death or significant complications if surgical intervention is used to manage their infection | • Diabetic foot infection at high risk of amputation despite conventional antibiotics • Aortic graft infection |
| Patient specific factors that preclude the use of conventional antibiotics | • Staphylococcus aureus osteomyelitis in patient with multiple antibiotic allergies • Some cystic fibrosis patients with nontuberculosis mycobacterial lung disease are unable to tolerate the side effects of antibiotic combination chemotherapy, which include severe nausea and risk of hearing impairment |